Confirmation
PR18: Anesthesia Induction
Applicable To
Introduction
Anesthesia Planning
In the context of BCEHS practice, planning for anesthesia is synonymous with planning for invasive airway management. Patients who are not completely obtunded will require some level of sedation and anesthesia prior to being intubated. Paramedics must consider multiple factors when planning an induction strategy.
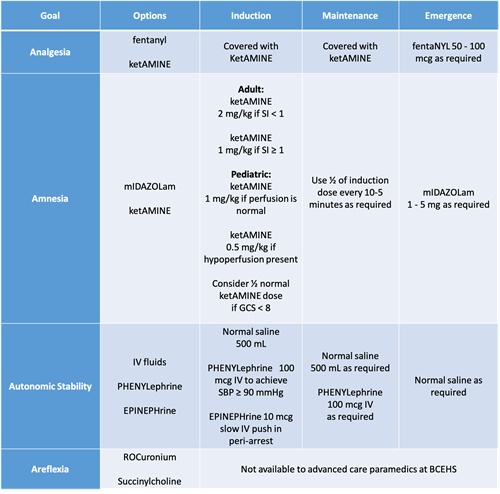
The goals of anesthesia, for all patients, are four-fold:
- Amnesia - Critical to the long-term psychological well-being of patients being intubated; can be achieved with the use of ketAMINE or mIDAZOLam.
- Analgesia - In addition to reducing patient discomfort, effective analgesia reduces the amount of sedation required post-intubation; can be achieved using ketAMINE and fentaNYL.
- Autonomic stability - Virtually all patients being intubated in the out-of-hospital setting require some degree of resuscitation during the peri-intubation phase. Hypotension post-intubation can be lethal. Autonomic stability can be achieved using fluid and push-dose vasopressors such as PHENYLephrine or EPINEPHrine.
- Areflexia - The loss of muscle tone and suppression of reflexes improves the overall ability of the intubator to access the trachea. Effective areflexia also lowers the total sedation requirements. It is, however, fraught with complications and can be extremely dangerous. Succinylcholine and rocuronium are used to achieve areflexia; deep sedation does not produce areflexia, but instead suppresses the response to painful stimulus.
Shock Physiology
Maintaining autonomic stability is critical to ensuring patient safety in the peri-intubation period. Because good outcomes cannot be achieved from a poor starting point, all patients must be adequately resuscitated prior to intubation. At a minimum, this involves a fluid bolus of normal saline of at least 500 mL.
The shock index (SI) is calculated by dividing the heart rate by the systolic blood pressure. Normal physiology has a shock index of less than 1; shocked states have an index of greater than 1. An approximation can be made by comparing the heart rate to the systolic blood pressure: if the heart rate is greater than the systolic blood pressure, the patient requires additional support during the peri-intubation phase. In these cases, PHENYLephrine as a push-dose vasopressor is used to help support blood pressure prior to and after intubation. EPINEPHrine is also available as a push-dose vasopressor for critically ill patients who are at imminent risk of cardiac arrest.
Summary of Pharmacology
Indications
Contraindications
- Absolute: inability to monitor oxygenation and ventilation
- Absolute: inability to perform airway interventions
- Relative: traumatic brain injuries
- Relative: hypotension and shock
Consider the use of alternative techniques (e.g., supraglottic airway devices, awake intubation techniques) if induction of anesthesia is judged unsafe, or if it cannot be accomplished due to logistical factors.
Procedure
- Ensure adequate oxygenation and ventilation throughout the procedure. Monitor pulse oximetry, blood pressure, and heart rate. Assign roles and delegate tasks as part of crew resource management. CliniCall consultation is required to discuss care planning options in patients with perfusing rhythms if clinical situation permits. Retrospective consultation is required post-intubation to support clinical decision-making and airway quality assurance.
- If not already done, establish vascular access and verify the line is patent.
- Prepare and label medications, including vasopressors, based upon shock index calculation. PHENYLephrine should be available at all times to manage post-intubation hypotension.
For adult patients
- Start normal saline bolus of 500 mL
- If shock index ≥ 1 (or predictors of hypotension are present):
- PHENYLephrine 100 mcg IV/IO every 3-5 minutes as required to maintain systolic blood pressure ≥ 90 mmHg
- ketAMINE 1 mg/kg IV/IO
- If shock index < 1:
- ketAMINE 2 mg/kg IV/IO
- For maintenance:
- ketAMINE: ½ of the induction dose every 10-15 minutes as required to maintain sedation
- fentaNYL: 50-100 mcg IV/IO every 10-15 minutes as required if pain is believed to be a major factor
- Normal saline: 250-500 mL as required
- PHENYLephrine: 100 mcg IV/IO every 3-5 minutes as required to a maximum of 500 mcg.
- CliniCall consultation required if additional PHENYLephrine is needed.
For pediatric patients
- Start normal saline bolus of 10 mL/kg
- If signs of inadequate perfusion are present - relative bradycardia; SBP < 70 + (2 x age):
- EPINEPHrine 1 mcg/kg slow IV/IO every 3-5 minutes as required
- ketAMINE 0.5 mg/kg IV/IO
- In patients with adequate perfusion and heart rate:
- ketAMINE 1 mg/kg IV/IO
- EPINEPHrine on “stand-by” 1 mcg/kg slow IV/IO every 3-5 minutes as required
- For maintenance:
- ketAMINE: ½ of the induction dose every 10-15 minutes as required to maintain sedation
- MIDAZOLam: consider addition of benzodiazepine at 0.1 mg/kg as required
- fentaNYL: consider 1-3 mcg/kg IV/IO every 10-15 minutes if pain is believed to be a major factor
- Normal saline: 10 mL/kg as required
- EPINEPHrine: 1 mcg/kg slow IV/IO as required