Confirmation
Download PDF
Open All
PR12: Intraosseous Cannulation
Applicable To
Introduction
Intraosseous cannulation is available as an option for paramedics requiring vascular access when peripheral attempts have failed.
Indications
PCP
- ⚠️ Requires completion of PCP scope expansion education:
- Following two unsuccessful peripheral IV attempts or an inability to visualize peripheral veins
- PCPs may attempt IO cannulation in patients in cardiac arrest ≥ 12 years old where there is a clear clinical history of hypovolemia, where fluid administration is a critical component of the resuscitation plan.
- -OR-
- IO’s may also be placed under direct supervision of a BCEHS ACP or higher
- The tibial site is the only site approved for PCP use. PCPs are limited to two collective attempts per patient only. Do not attempt to re-cannulate a site that has failed or been dislodged.
ACP
- Following two unsuccessful peripheral IV attempts or an inability to visualize peripheral veins (including external jugular vein)
- Unstable patient requiring medications or fluid replacement
- Important considerations:
- The ACP (or higher) remains responsible for any anesthesia or pain management requirements.
- Intraosseous placement must not delay or impair the delivery of high-quality CPR, effective airway management, or defibrillation. Placement should be deferred until at least three rounds of chest compressions, with AED analyses, have been completed.
Contraindications
- Skeletal or tissue damage in the extremity to be used
- Prior proximal tibial surgery or knee joint replacement
- Signs of infection around the site
- Intraosseous placement at the same site in previous 48 hours
- PCP: Not authorized for use in patients under 12 years of age (aligns with restrictions on IV initiation)
Procedure
- Assemble equipment, including EZ-IO driver, needle, primed EZ-Connect extension, infusion fluid and line set, and 10 mL syringe of normal saline.
- Select the site of needle insertion and clean the skin.
- Using aseptic techniques, drive the needle into the bone. Press gently: let the drill do most of the work.
- Remove the stylet and securely discard the sharp. Place the stabilizer dressing over the needle hub.
- Connect a primed EZ-Connect extension.
- ACP (or PCP under direction of an on-scene ACP): In patients who are conscious, prime the EZ-Connect extension with lidocaine - see step 7.
- Aspirate for the presence of bone marrow or blood to confirm the placement. If patent, connect the IV tubing to the EZ-Connect extension set. If unsuccessful, change to another site on a different limb. Do not reuse the same limb.
- ACP (or PCP under direction of an on-scene ACP): In patients who are conscious, administer lidocaine, 40 mg (0.5 mg/kg in children to a maximum of 40 mg)
- Instill the lidocaine slowly, over 120 seconds, making sure to administer the appropriate amount of lidocaine through the extension, and allow it to dwell in the bone marrow for 60 seconds.
- Slowly flush the IO with 5-10 mL normal saline (2-5 mL in children) following the administration of lidocaine.
- Connect the 10 mL syringe to the proximal access port on the IV tubing. Flush the line and the extension set, pushing firmly and briskly on the syringe plunger.
- Set the appropriate flow rate. Pressure infusers or intermittent boluses may be required.
- Protect the site and monitor for signs of extravasation.
Notes
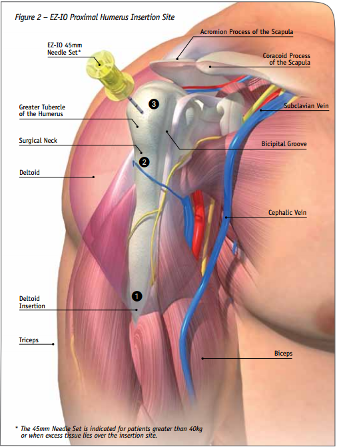
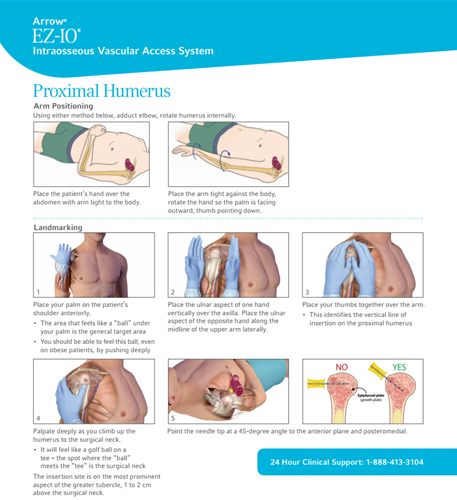
- Needle placement in the proximal humerus has been demonstrated to have significantly improved infusion rates compared to the tibial plateau. It should be considered as the preferred IO site in patients under ACP care. If using the humerus, choose the larger (yellow) needle. To review anatomy and landmarks, see video below.
- Tibial placement is the only permissible insertion site for PCPs.

- Paramedics should review this educational material for additional information about intraosseous site selection. Contact a Paramedic Practice Educator for specific questions or concerns.
- Intraosseous catheters are approved for use in patients for up to 24 hours when placed in the proximal humerus and both the proximal and distal tibia. It may be extended for up to 48 hours in patients over the age of 12 under exceptional circumstances.
Resources

Tibial placement:
Humeral landmarking:
References
- 2024-05-01: updated PCP scope information
- 2023-09-29: added PCP scope information