Confirmation
CP 4.23: Wound Care
PURPOSE
The purpose of this Community Paramedicine Wound Care Clinical Practice Guideline is to support Community Paramedics (CP) in playing an active role in the early identification and assessment of those at risk of, or experiencing, skin breakdown.
The role of Community Paramedic skin and wound care education and training focuses on understanding the phases of wound healing, including the barriers to healing; conducting a comprehensive wound assessment; identifying wound management goals; and selecting dressings that support moisture balance, infection control, and pain management strategies.
CPs utilize their skills to identify and manage common wounds, including;
- skin tears
- pressure injuries
- diabetic foot ulcers
- venous and arterial leg ulcers
- surgical wounds
CPs can also differentiate between local and systemic wound infections.
Community Paramedics can;
- Conduct routine skin evaluation and identify early signs of skin breakdown,
- Provide independent or collaborative wound care for superficial wounds above the level of the dermis, non-infected wounds with less than 25% necrosis and minimal or no drainage,
- Escalate the care of deteriorating or non-healing wounds to community care nursing teams, regional NSWOCs, or Primary Care Providers for evaluation and wound care planning development.
- Support patients with more complex wounds, provided that wound care treatment plans are created, led, and frequently and routinely reassessed per the care plan by Community Health Nurses, Regional NSWOC, or Primary Care Providers.
POLICY STATEMENTS
Prior to undertaking any independent or collaborative wound assessment or wound care, Community Paramedics who are in good standing with BC Emergency Health Services Community Paramedic Program, and whose names appear on the BCEHS Community Paramedic registry, must first complete the 30-hour WOC Canada Community Paramedic Skin and Wound Course, and the full-day in-person training session led by a WOC-contracted, BC-based NSWOC, as well as the Community Paramedic Wound Care Documentation course. Verification of successful completion of these three elements must be verifiable by the Community Paramedic Program Team.
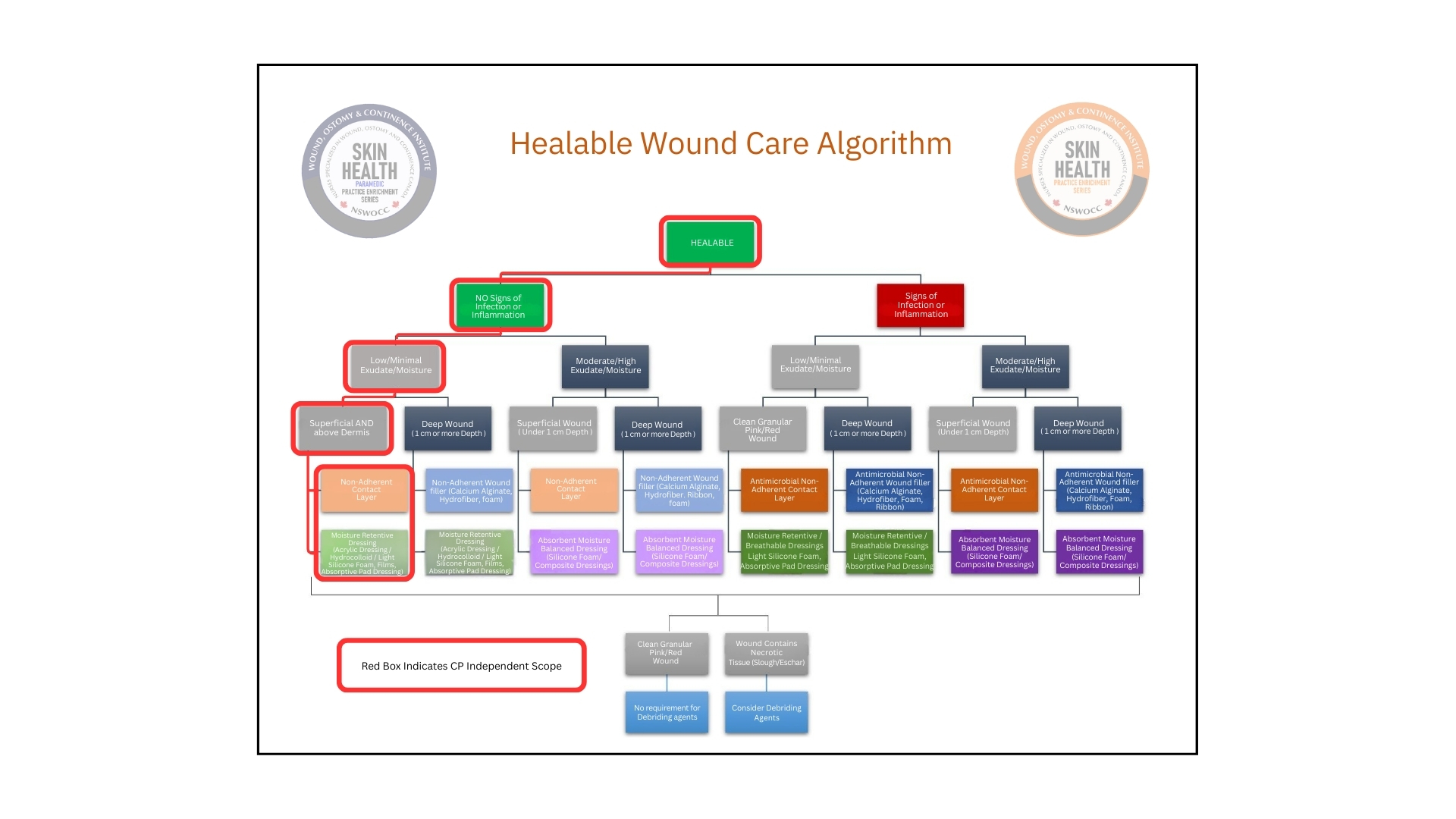
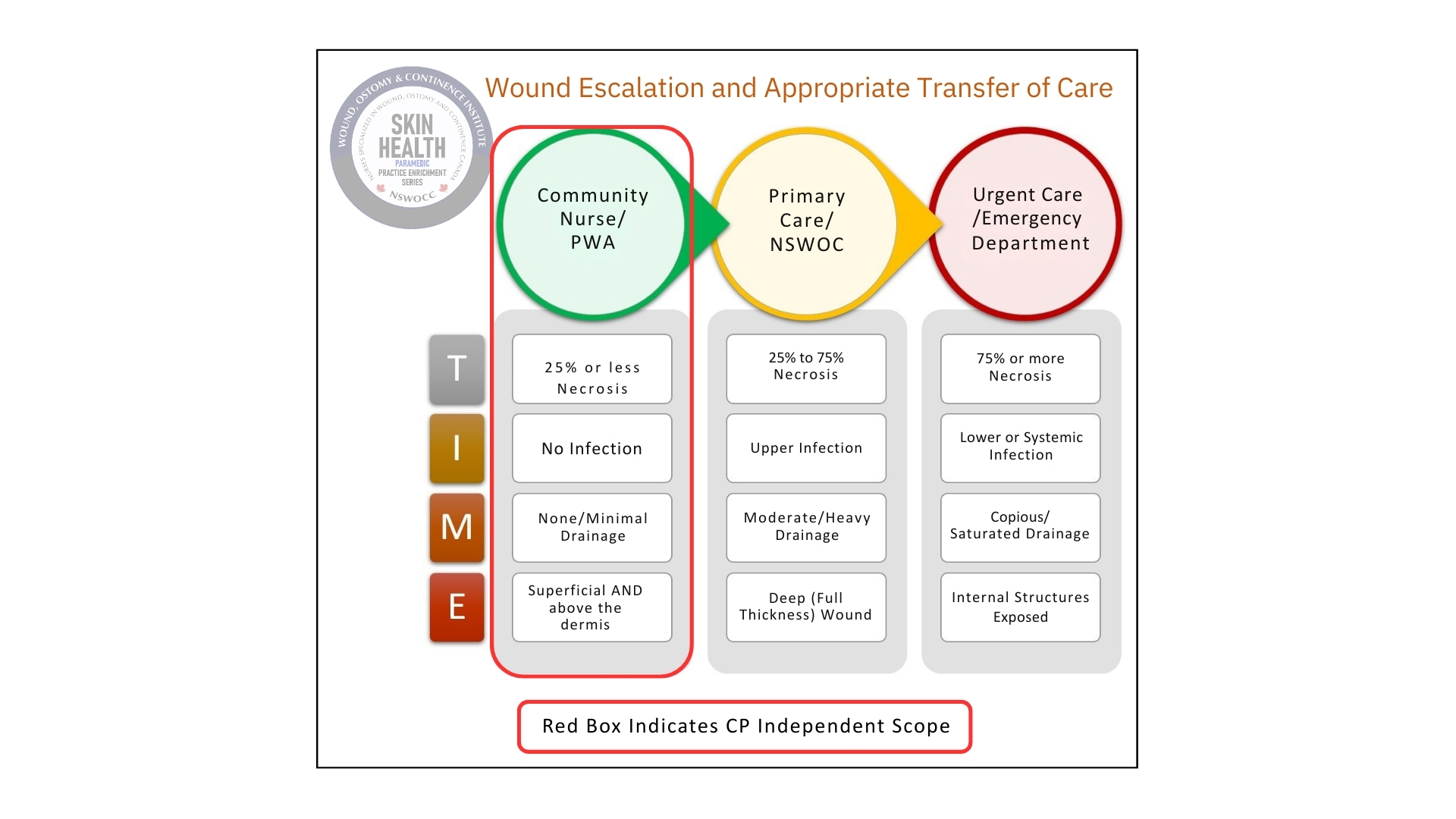
The independent management of wounds by Community Paramedics is limited to the left-most column in the WOC Institutes’ “Wound Escalation and Appropriate Transfer of Care” table (PWA = Paramedic Wound Associate), circled in red, and the left-most steps in the decision tree of the “Healable Wound Care Algorithm”, also circled in red.
SCOPE OF PRACTICE
Note that the areas one the NSWOC Images circled in red are within the scope of a Community Paramedic for management.
Wound presentations outside the highlighted area require wound care treatment planning to be developed, led, and routinely reassessed by Community Nursing, NSWOC, or Primary Care Teams.
CPs may supplement the wound care provided in these situations, provided they have adequate orientation to the specific wound care needs and adequate knowledge and understanding of the procedure and products to safely provide the requested care.
Any concern regarding the deterioration of a client’s skin, wound, or any progression to systemic illness must result in immediate notification to community care team members and/or regional NSWOC involved in the patient’s care, as well as to the patient’s most responsible provider (MRP), or overseeing specialist (plastic surgeon, infectious disease doctor).
GUIDELINE OUT OF SCOPE FOR CP'S
Wound care provided by CP must NEVER include;
- negative pressure therapy devices,
- wound debridement,
- incision and/or drainage,
- suturing, stapling, or gluing of tissue,
- removal of sutures, staples or other skin closure devices,
- care of stomas,
- care of indwelling tubes, lines or drains
- packing of wounds where the wound bed is not visible
- packing of wounds deeper than the dermis layer
- initiation or application of compression therapy
PRODUCTS
Community Paramedics may only provide independent wound care using the equipment provided to them by BCEHS. This includes;
- Sterile dressing tray (forceps, gauze, garbage bag, sterile field drape)
- Sodium chloride 0.9%
- Sterile Water
- Sterile single-use scissors
- Sterile single-use cotton-tipped wound probe and measuring ruler
- Iodine impregnated mesh dressing (e.g. Inodine)
- Non-adherent petroleum impregnated dressing (e.g. Adaptic)
- ABD pads
- Cling Gauze bandages
Refer to the wound care product sheet for the appropriate use of these types of dressings.
- Inadine - https://www.clwk.ca/get-resource/inadine/
- Adaptic - https://www.clwk.ca/get-resource/adaptic/
Collaboration with Community Nurses and NSWOCs may include other dressing types provided by these teams. The appropriate use of these dressings must be clearly outlined in the client’s documented wound care plan. Community Paramedics must ensure they are familiar with each wound care product and its appropriate use before its use.
Wound Care Product Information can be found here: https://www.clwk.ca/groups/product-information-sheets/custom/?cf_id=1910&cof_id=1814
DOCUMENTATION
When available, Community Paramedics will document all wound care provided in the client’s Pixalere file. An ePCR must also be created for each client visit, and if wound care is provided during this visit, the Pixalere file number must be included in the ePCR documentation.
When Pixalere is not available, wound assessments and any wound care that is provided by a CP will be documented on a patient-specific Wound Assessment and Treatment Flowsheet (WATFS) and included in a mandatory SIREN ePCR, as well as forwarded to any and all involved Community Health teams or requesting regional NSWOC within the patient’s circle of care. Wound care documentation must be completed and relayed to the appropriate care teams on the same day the wound assessment and care are provided.